June 29, 2009
The numbers of anesthesiologists reported to the National Practitioner Data Bank (NPDB), which was created by the Health Care Quality Improvement Act of 1986 (HCQIA), continue to be very low. Anesthesiologists accounted for only 7,370 of a total of 234,747 malpractice payment settlements reported to the NPDB between 1990 and 2007 (3 percent). The numbers of nurse anesthetists thus reported are even lower. Plaintiffs’ lawyers tend to target the deep pockets and hospitals and physicians much more readily than they sue nurses. Only 2.1 percent of all malpractice payment reports were for nurses, according to the 2006 NPDB Annual Report, and only 19 percent of the 2.1 percent were attributable to anesthetists.
Physicians, but not nurse anesthetists or other allied health providers, are also the subject of mandatory reporting by hospitals that take adverse licensure, privileging or professional society membership actions them.
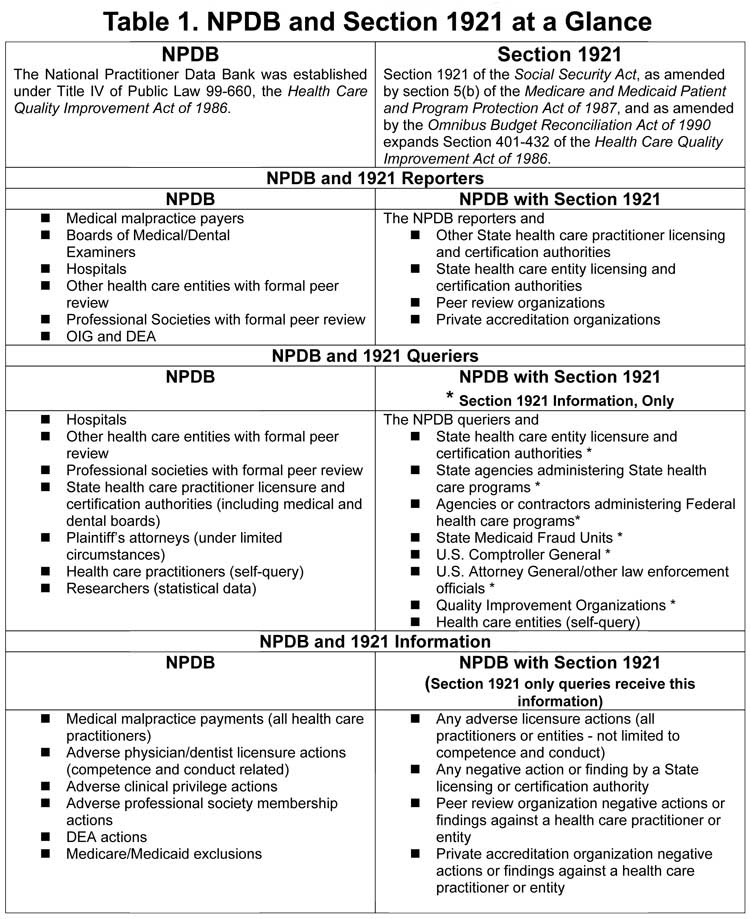
Although 1987 legislation amended Section 1921 of the Social Security Act and expanded NPDB activities to include all licensed health care practitioners and entities, the regulations required for implementation have not been finalized (after 12 years!). Upon implementation of Section 1921 – final regulations are expected this year -- hospitals will have the option of reporting adverse actions affecting the clinical privileges of non-physician providers.
Hospitals are beginning to adopt codes of conduct granting them the power to discipline physicians for “inappropriate behaviors,” as required by the new Joint Commission leadership standard (LD.03.01.01). Some of these codes of conduct give the hospitals considerable leeway in removing “disruptive” physicians” from the medical staff or engaging in economic credentialing. (See Alert dated May 11, 2009.) Because of the potential risk of increasing numbers of reports to the NPDB, a mini-refresher course on the NPBD program may be helpful to our readers.
Table 1 compares the current version of the NPDB to the NPDB as amended by Section 1921, in the proposed implementing regulations.
Looking at Table 1, we can see that fraud and abuse may be reported to the NPDB if it results in exclusion from the Medicare/Medicaid program by the Office of the Inspector General (OIG). Other types of fraud and abuse information are contained in the Healthcare Integrity and Protection Data Bank (HIPDB), which was mandated by the Health Insurance and Portability Act of 1996 (HIPAA). In the current climate of intensifying fraud and abuse scrutiny, it is worth familiarizing (or re-familiarizing) ourselves with the HIPDB.
The HIPDB went into operation in 2000. The specific, focused intent was to combat fraud and abuse in the healthcare industry. Of particular note, the HIPDB stores reports of civil judgments as well as criminal convictions of practitioners, providers and suppliers “related to the delivery of a health care item or service –‘ and the information is available to private health plans. Table 2 shows the overlaps and differences between the HIPDB and the NPDB with implementation of Section 1921.
To make it easier and speedier than ever to track practitioners’ errors, accidents or fraud and abuse, the federal agency responsible for the NPDB and HIPDB are encouraging organizations that use the data banks to enroll their practitioners in the Proactive Disclosure Service Prototype (PDS). As the July 2009 issue of NPDB-HIPDB Data Bank News says, “Using PDS helps to ease the credentialing process by automatically notifying you of new or changed reports on enrolled practitioners within 24 hours of receipt by the Data Banks. You receive notification of new reports without having to do a traditional query on the practitioner.”
We sympathize with our readers who are feeling besieged. We hope that “At least to know the worst is sweet,” as Emily Dickinson wrote in Rouge Gagne. Please watch your inboxes for further information on the Recovery Audit Contractors (RACs) and other enforcement efforts, and, as always, let us know if you have questions.
Sincerely,
Tony Mira
President and CEO